A T2D treatment approach that prioritizes weight management in support of glycemic control may result in more comprehensive T2D management.1,2,3
In patients with T2D and overweight or obesity, weight loss can be associated with improvement in glycemic control. In the Look AHEAD (Action for Health in Diabetes) study evaluating intensive lifestyle intervention (ILI) in comparison to conventional care, participants in the ILI group were more likely to lose weight and also more likely to achieve ancillary benefits of decreased medication use.4-7
Findings from the Look AHEAD trial
The Look AHEAD trial examined the long-term effects of lifestyle interventions on cardiovascular (CV) morbidity and mortality in 5145 adults with T2D and overweight or obesity who received ILI or diabetes support and education (DSE). The trial was stopped due to futility analysis, with no demonstrated significant intergroup difference in the primary CV outcome.2,7,8*
*Primary eligibility criteria: being aged 45-76; having a BMI ≥25 kg/m2 (≥27 kg/m2 if treated with insulin), systolic and diastolic blood pressure <160/100 mm Hg (with or without antihypertensive drugs), and triglycerides <600 mg/dL (with or without drugs for dyslipidemia); and successful completion of a valid maximal-graded exercise test.2,7
1-year data demonstrated significant changes in multiple study measures in the ILI group compared with the DSE group7
- 19.18 lb weight loss vs 1.76 lb reductions in the DSE group5
-
The ILI group demonstrated a significant reduction in waist circumference (P<0.001); however, the mean waist circumference remained in the range of abdominal obesity7
- Waist circumference is an indirect measure of abdominal adiposity9
- Significantly lower A1C levels (P<0.0001), with the ILI group, on average, achieving an A1C level in the target range of <7%5
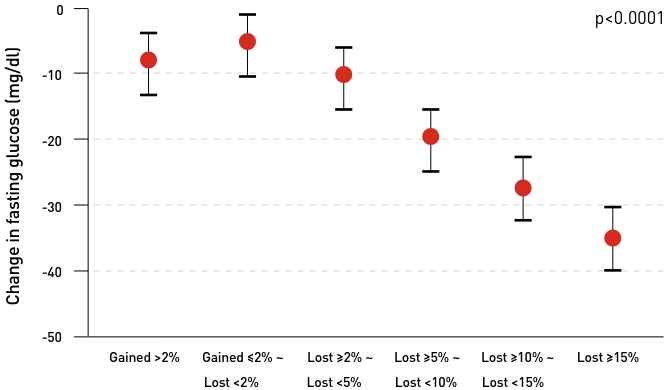
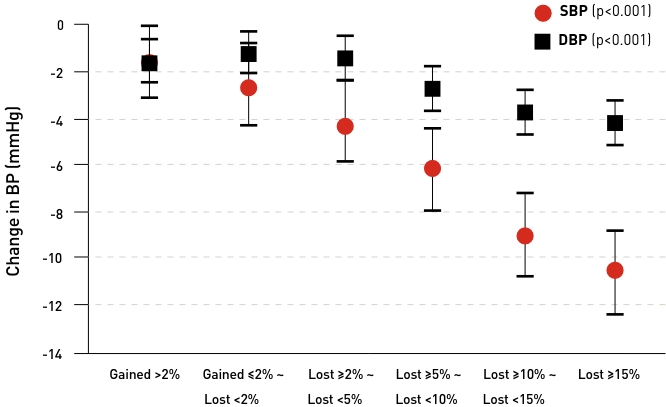
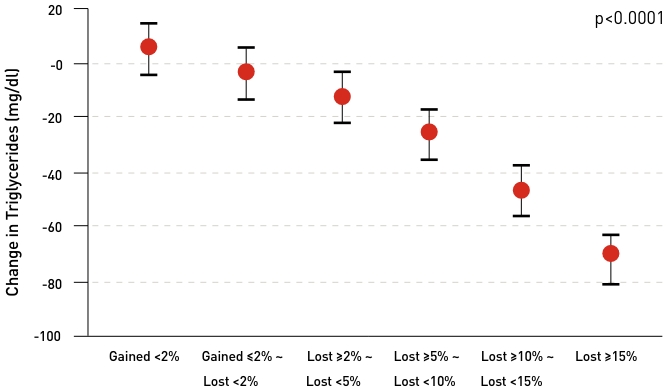
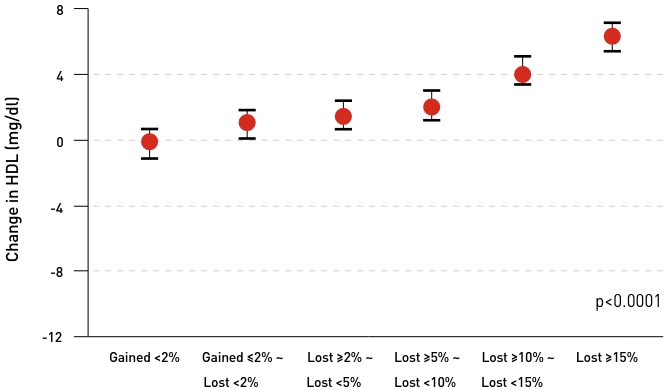
Weight loss from ≥2% to ≥15% is associated with significant improvements in T2D-related risk factors:
According to the American Diabetes Association, modest and sustained weight loss may reduce the need for additional medications in patients with T2D and obesity.3
In patients with T2D and obesity, modest and sustained weight loss leading to clinically meaningful improvements in glycemic control, lipids, and blood pressure may reduce the need for additional medications to control these risk factors.
- Weight loss of 5% to 10% confers metabolic improvement13
- Weight loss of 10% to 15% or more can have a disease-modifying effect and lead to remission of diabetes13*
*Defined in a 2022 consensus report as normal blood glucose levels for 3 months or more in the absence of pharmacological therapy.13
The benefits of early intensive glucose lowering have been well established.13 Prioritizing weight management can support early glycemic control.5
According to the UK Prospective Diabetes Study (UKPDS),* early intensive glycemic control (A1C <7%) has been associated with reducing the long-term risk of complications in patients with T2D (compared to conventional care at the time of the study).14,15
Participants in the intervention group with newly diagnosed T2D maintained a lower median A1C over 10 years of 7.0% compared with 7.9% in the control group. Early intensive glycemic control† led to:




Benefits to microvascular complications, diabetes-related endpoints, diabetes-related death, and all-cause mortality continued to be demonstrated after 10 years14
Please note that weight loss was not part of the UKPDS trial. On average, participants in the UKPDS trial gained weight, potentially associated with the use of sulfonylureas and insulin.14
*The UK Prospective Diabetes Study (UKPDS) was designed to evaluate whether intensive blood glucose control reduced the risk of vascular complications. Between 1977 and 1991, 3867 eligible patients (newly diagnosed with type 2 diabetes, 25 to 65 years of age, with a fasting plasma glucose level >6 mmol/L on 2 mornings, 1-3 weeks apart) were randomly assigned to an intensive regimen with treatment or a conventional regimen with diet. The exclusion criteria were: ketonuria more than 3 mmol/L; serum creatinine greater than 175 μmol/L; myocardial infarction in the previous year; current angina or heart failure; more than 1 major vascular event; retinopathy requiring laser treatment; malignant hypertension; uncorrected endocrine disorder; occupation that precluded insulin therapy; severe concurrent illness that would limit life or require extensive systemic treatment; inadequate understanding; and unwillingness to enter the study14
†Early intensive glycemic control was with sulfonylureas, insulin, or metformin compared with conventional dietary therapy.14
The DiRECT: Diabetes Remission Clinical Trial*
Glycemic control was assessed in participants with T2D (≤6 years), 20 to 65 years of age, who were provided either a structured weight-management program (intervention group) or diabetes management per current best practices. Additionally, patients in the intervention group had all antihyperglycemic and antihypertensive medications withdrawn at baseline.6
- Structured weight management intervention led to a greater proportion of participants achieving glycemic control: at the 2-year follow-up, an A1C <6.5% was achieved by 36% of participants in the intervention group vs 3% of participants in the control group.
-
Benefits related to reduction in medication use were also demonstrated.
- At the 2-year follow-up, 60%* of participants in the intervention group were not taking any antidiabetic medications vs 16% in the control group.6
*40% of participants in the intervention group required medications; 84% in the control group required medications. This statement reflects calculated values from Lean MEJ, et al.6
In year 2 of this analysis, participants with greater maintained weight loss were more likely to have an A1C <6.5%, as demonstrated in a post hoc analysis of the entire study population (pooled intervention and control participants) by weight-loss category. In this analysis, an A1C <6.5% was achieved by6:



*DiRECT (Diabetes Remission Clinical Trial) was a 2-year, open-label, cluster-randomized controlled trial designed to assess remission of type 2 diabetes during a primary care-led weight-management program, as well as the durability of the intervention effect. 149 patients were included in the intervention group, 149 in the control group. Eligible participants were aged 20-65 years, had been diagnosed with type 2 diabetes within the previous 6 years, and had a BMI of 27-45 kg/m2. Exclusion criteria included current insulin use, A1C of 12% or higher, weight loss of more than 11 lb within the previous 6 months, and a recent recorded estimated glomerular rate of less than 30 mL/min per 1.732 m2.6
Treating excess weight in T2D is a component of a patient-centered approach that, if started early, can support early glycemic control.3,13
- Collaboration between patients with T2D and physicians can help improve the clinician-patient relationship.
-
Positive interactions with physicians can help circumvent negative health and behavioral consequences of patient experiences with weight stigma.16,17
- Combating negative weight-based stereotypes held by staff can help shift the clinical culture away from stigmatizing patients and toward empowering them in their health-improvement efforts.17
- Not using motivational interviewing and other nonjudgmental, patient-centered communication approaches predicts lower patient adherence, patient-provider trust, and patient outcomes.17
Patients with T2D and excess weight may benefit from formal medical support.1
- Weight management may support improved glycemic control and a reduction in multiple risk factors in patients with T2D.
- Therefore, to achieve early glycemic control, physicians should offer both education and weight-management support to all people with T2D and overweight or obesity upstream in the treatment continuum.
According to the American Diabetes Association providers should3


It is important to consider the effect of glucose-lowering medications on weight for patients with T2D and overweight or obesity.
Starting conversations about weight can be challenging for both HCPs and patients. For examples of a collaborative approach and questions that can start these sensitive conversations, watch the Let’s TALK! short videos in the Resource Hub.

- Tina’s doctor acknowledged that maintaining weight loss is a challenge and praised her efforts.
- This set Tina at ease, as she felt that her hard work was being recognized, even though she had experienced weight regain.
- Tina and her doctor discussed her weight-loss goals, focusing on improving glycemic control and her diabetes-related health.
- Once they aligned on goals, her doctor helped her set some specific, measurable, and attainable objectives around diet and exercise, including tracking her food intake using a diary and exercising 3 times a week.
- Her doctor gave her a referral to a dietitian for additional support and promised to continue checking in on her, which helped to motivate Tina.
Medical Workmat
Conversations about weight management in patients with T2D can be challenging. Download the Medical Workmat from the Resource Hub to help navigate those conversations.
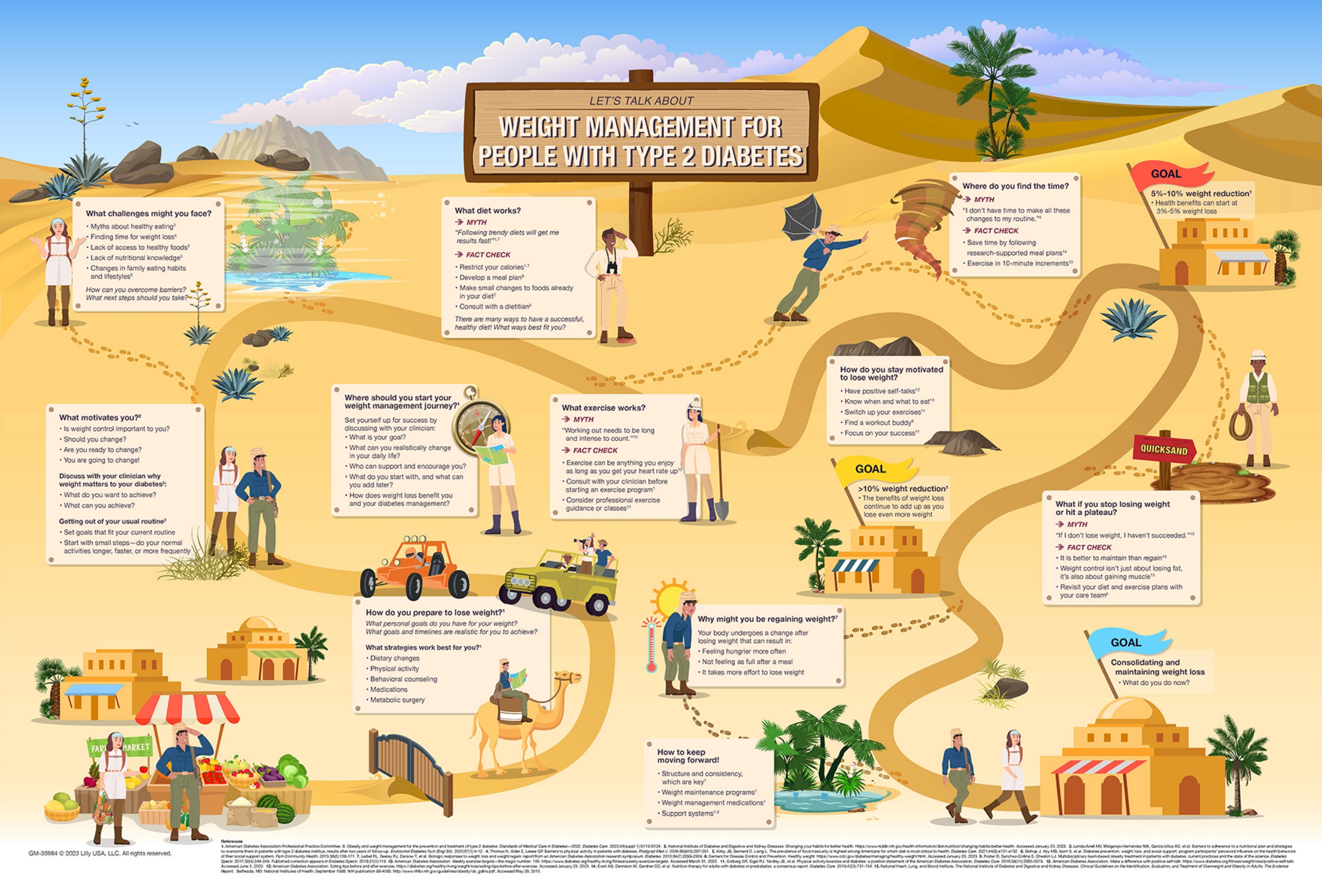
Weight management early in the course of diabetes care targets a key component of diabetes pathophysiology.1,6
Early Weight Management is an Important Upstream Intervention in T2D Care1,6
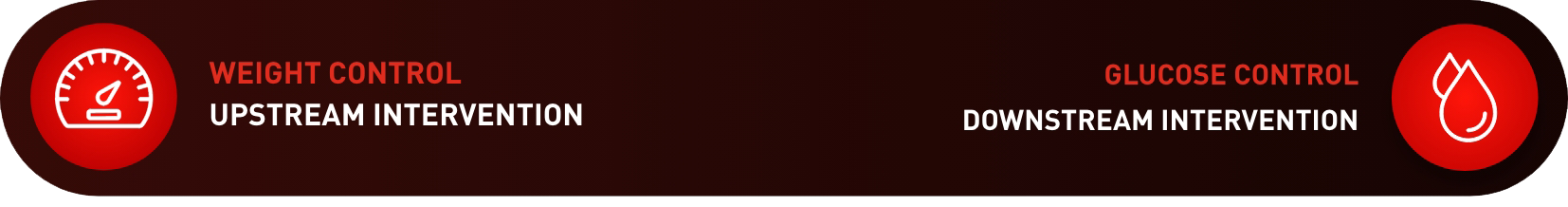
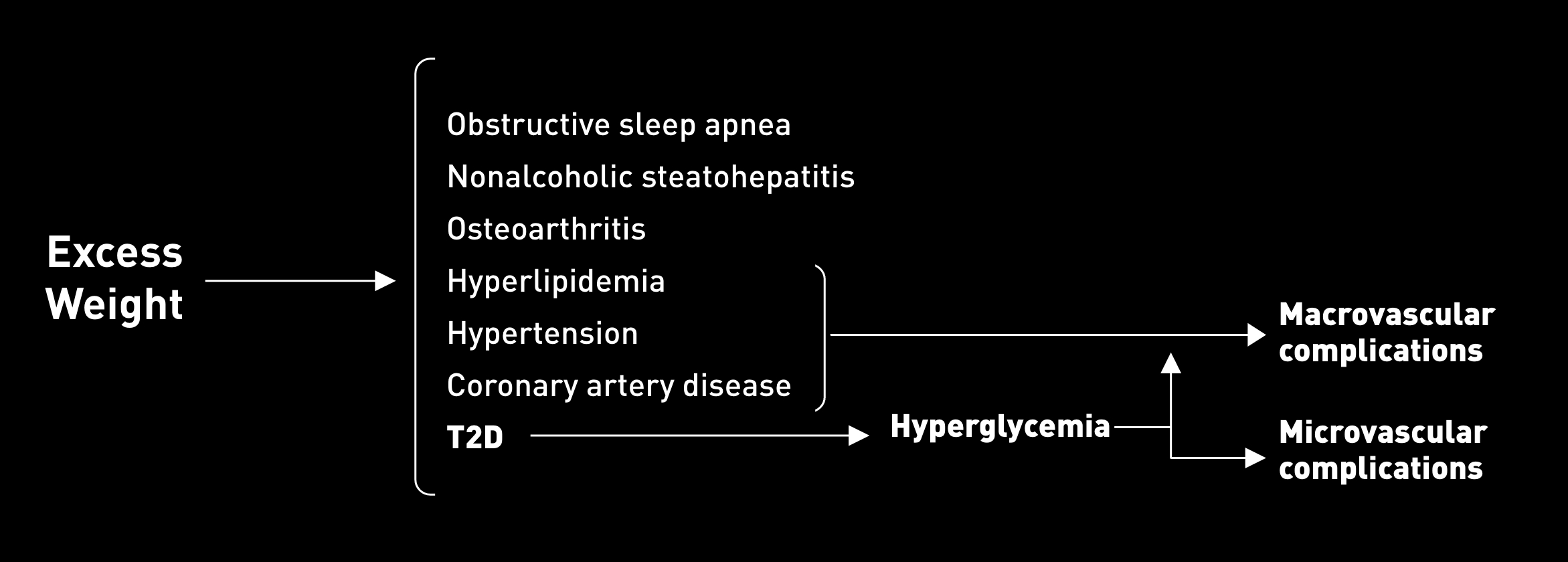
For patients with T2D, a treatment approach that addresses excess weight upstream could provide more clinical benefit than one that focuses exclusively on glycemic control.1,8
You have resources when it comes to excess weight in T2D.
STAY INFORMED. VISIT THE RESOURCE HUB FOR EXCESS WEIGHT IN T2D RESOURCES HUB.
T2D=type 2 diabetes.
References
- Lingvay I, Sumithran P, Cohen RV, le Roux CW. Obesity management as a primary treatment goal for type 2 diabetes: time to reframe the conversation. Lancet. 2022;399(10322):394-405. doi:10.1016/S0140-6736(21)01919-X.
- Look AHEAD Research Group. Effect of a long-term behavioural weight loss intervention on nephropathy in overweight or obese adults with type 2 diabetes: a secondary analysis of the Look AHEAD randomised clinical trial. Lancet Diabetes Endocrinol. 2014;2(10):801-809. doi:10.1016/S2213-8587(14)70156-1.
- American Diabetes Association Professional Practice Committee. 8. Obesity and weight management for the prevention and treatment of type 2 diabetes: standards of medical care in diabetes-2024. Diabetes Care. 2024;47(suppl 1):S145-157. doi:10.2337/dc24-S008.
- Wing RR, Lang W, Wadden TA, et al. Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care. 2011;34(7):1481-1486. doi:10.2337/dc10-2415.
- Redmon JB, Bertoni AG, Connelly S, et al. Effect of the Look AHEAD study intervention on medication use and related cost to treat cardiovascular disease risk factors in individuals with type 2 diabetes. Diabetes Care. 2010;33(6):1153-1158. doi:10.2337/dc09-2090.
- Lean MEJ, Leslie WS, Barnes AC, et al. Durability of a primary care-led weight-management intervention for remission of type 2 diabetes: 2-year results of the DiRECT open-label, cluster-randomised trial. Lancet Diabetes Endocrinol. 2019;7(5);344-355. doi:10.1016/S2213-8587(19)30068-3.
- Look AHEAD Research Group. Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes [published correction appears in N Engl J Med. 2014;370(19):1866]. N Engl J Med. 2013;369(2):145-154. doi:10.1056/NEJMoa1212914.
- The Look AHEAD Research Group. Eight-year weight losses with an intensive lifestyle intervention: the Look AHEAD study. Obesity (Silver Spring). 2014;22(1):5-13. doi:10.1002/oby.20662.
- Grundy SM, Neeland IJ, Turer AT, Vega GL. Waist circumference as measure of abdominal fat compartments. J Obes. 2013;454285. doi:10.1155/2013/454285/10.1155/2013/454285.
- Grandy S, Fox KM, Hardy E. Association of weight loss and medication adherence among adults with type 2 diabetes mellitus: SHIELD (Study to Help Improve Early evaluation and management of risk factors Leading to Diabetes). Curr Ther Res Clin Exp. 2013;75:77-82. doi:10.1016/j.curtheres.2013.06.004.
- Gordon J, McEwan P, Idris I, Evans M, Puelles J. Treatment choice, medication adherence and glycemic efficacy in people with type 2 diabetes: a UK clinical practice database study. BMJ Open Diabetes Res Care. 2018;6(1):e000512. doi:10.1136/bmjdrc-2018-000512.
- Egede LE, Gebregziabher M, Echols C, Lynch CP. Longitudinal effects of medication nonadherence on glycemic control. Ann Pharmacother. 2014;48(5):562-570. doi:10.1177/1060028014526362.
- Davies MJ, Aroda VR, Collins BS, et al. Management of hyperglycemia in type 2 diabetes, 2022. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2022;45(11):2753-2786. doi.org/10.2337/dci22-0034.
- UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998;352:837-853. doi:10.1016/S0140-6736(98)07019-6.
- Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008;359(15):1577-1589. doi:10.1056/NEJMoa0806470.
- Puhl RM, Himmelstein MS, Hateley-Browne JL, Speight J. Weight stigma and diabetes stigma in U.S. adults with type 2 diabetes: associations with diabetes self-care behaviors and perceptions of health care. Diabetes Res Clin Pract. 2020;168:108387. doi:10.1016/j.diabres.2020.108387.
- Puhl RM, Phelan SM, Nadglowski J, Kyle TK. Overcoming weight bias in the management of patients with diabetes and obesity. Clin Diabetes. 2016;34(1):44-50. doi:10.2337/diaclin.34.1.44.