Many patients with T2D struggle to achieve and maintain meaningful weight loss.1-7
T2D and weight loss: Even in an optimal clinical trial setting, intensive lifestyle intervention (ILI) does not achieve weight loss for all participants with T2D and excess weight. The Look AHEAD trial* evaluated participants receiving ILI and ongoing monthly support compared to participants only receiving standard of care.
Maintenance of initial weight loss was a challenge for many patients.

*The Look AHEAD (Action for Health in Diabetes) study assessed the effects of weight loss achieved through intensive lifestyle intervention (ILI) on cardiovascular (CV) morbidity and mortality. A total of 5145 eligible adult men and women 45 to 76 years of age with type 2 diabetes and a body mass index (BMI) ≥25 kg/m2 (BMI ≥27 kg/m2 in participants taking insulin) were randomly assigned to ILI or usual care (ie, diabetes support and education) over 8 years. The trial was stopped due to futility analysis with no demonstrated significant intergroup difference in the primary CV outcome.6
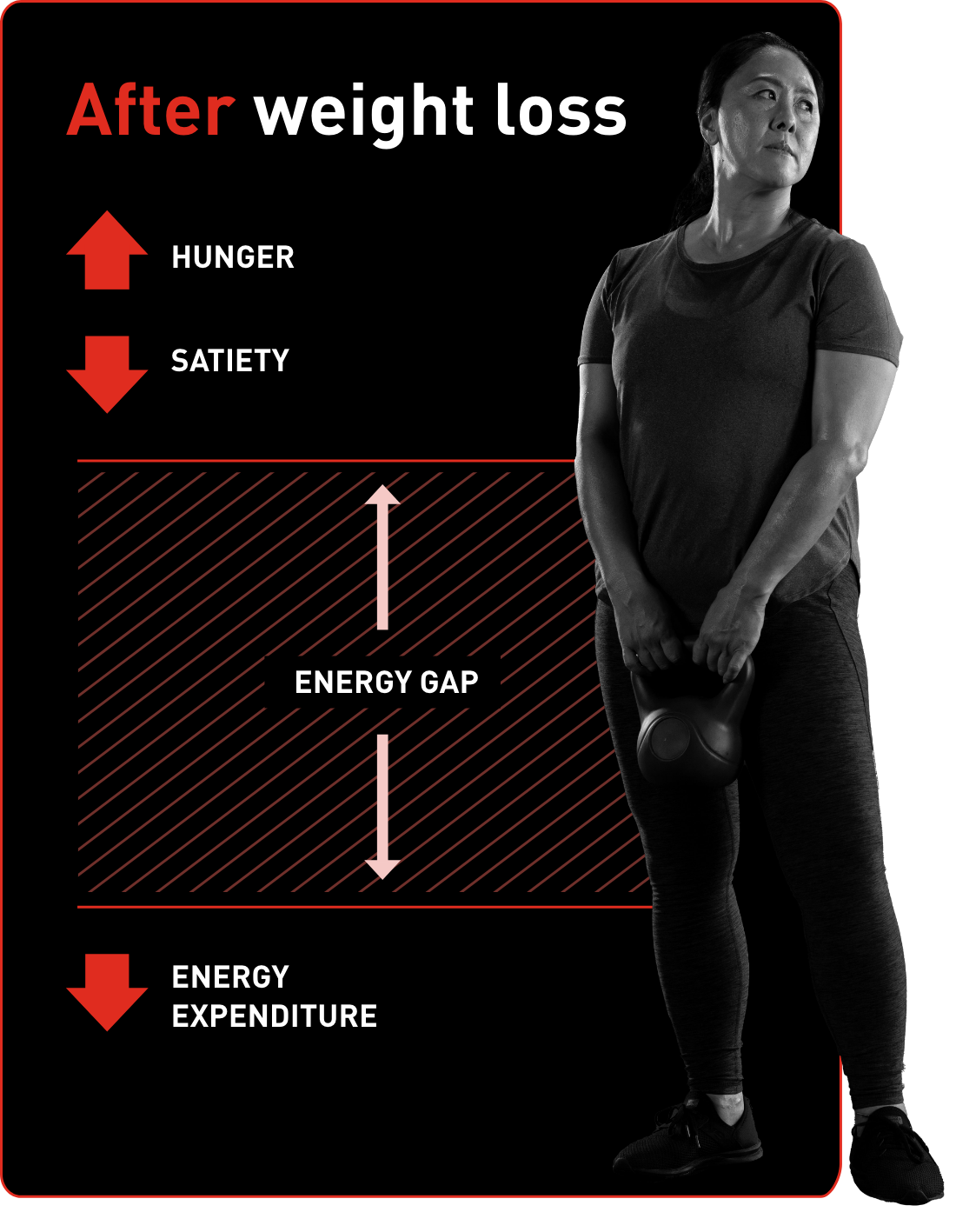
Metabolic adaptation can present an additional challenge for patients with T2D and excess weight.8-11
Metabolic adaptation is an adaptive hormonal and metabolic response associated with weight loss through diet and exercise, which results in a tendency toward weight regain.

- Hormonal changes identified in patients with obesity who achieve initial weight loss have also been seen in patients with T2D and overweight/obesity who undergo a lifestyle intervention associated with weight loss, supporting the presence of these same mechanisms of metabolic adaptation.
- This evidence comes from a post hoc analysis of the DiRECT study,* which investigated whether appetite-related hormones were predictors of weight regain. Data were available for 253 individuals (147 interventions, 106 controls) with T2D (age 53.6 ± 7.5 years, BMI 34.7 ± 4.4 kg/m2, 59% men). Intervention participants received a 24-month weight-management program, and the control group remained on usual diabetes care.
This is based on research in healthy humans with overweight or obesity but has also been demonstrated among participants with T2D.
*DiRECT (Diabetes Remission Clinical Trial) was a 2-year, open-label, cluster-randomized controlled trial designed to assess remission of type 2 diabetes during a primary care-led weight-management program, as well as the durability of the intervention effect. 149 patients were included in the intervention group, 149 in the control group. Eligible participants were aged 20-65 years, had been diagnosed with type 2 diabetes within the previous 6 years, and had a BMI of 27-45 kg/m2. Exclusion criteria included current insulin use, A1C of 12% or higher, weight loss of more than 11 lb within the previous 6 months, and a recent recorded estimated glomerular rate of less than 30 mL/min per 1.732 m2.12
Hormonal changes as a result of weight loss can be associated with weight gain8,9
Weight loss can trigger an imbalance resulting in chronic increase in ghrelin (leading to increased hunger) and a decrease in leptin (decreased satiety), while the energy expenditure is reduced due to a reduction in body weight and food intake, among other mechanisms. This imbalance between desired energy and required energy results in an energy gap that can make it challenging to achieve and maintain weight loss.8,9
Following a rigorous diet and exercise regimen, Tina lost 9 lb in 6 months—about 5% of her baseline weight.
- She then stopped exercising as often but still experienced increased feelings of hunger, accompanied by intermittent overeating.
- Tina was unable to maintain her weight loss, regaining the 9 lb in 2 months.
- After Tina regained the weight, her blood sugar regulation was affected: she saw her A1C increase by 0.3% at her next doctor’s appointment.
Weight bias may impact T2D care4
Conscious or unconscious weight bias may influence how some clinicians manage care of patients with T2D who have excess weight. This is often associated with:
- Elevated diabetes-specific emotional distress
- Less involvement from the patient in treatment decisions
- Fewer clinician-patient communications
Need help with conversations about excess weight in T2D management? See the RESOURCE HUB FOR EXCESS WEIGHT IN T2D.
The relationship between weight and T2D medications can be complex
A treatment approach that includes consideration of how a medication can affect weight may provide more benefit than one exclusively focused on glycemic control.6,9,16,17
Studies have shown that some antihyperglycemic agents may be associated with weight gain3,18
Based on a review by Apovian et al., summarizing the weight-related effects of widely used classes of antihyperglycemic agents on body weight in patients with T2D, multiple classes of diabetes therapy may be associated with weight gain.18
Hear from experts in diabetes care
Dr. Alice Cheng, Associate Professor at University of Toronto, Canada, shares why it is important to address excess weight as part of comprehensive T2D management and how to approach this in a sensitive and collaborative way with your patients.
Now that potential barriers have been identified, review the benefits of early action in Early Glycemic Control and Weight Management in T2D.
T2D=type 2 diabetes.
References
- Franz MJ. Weight management: obesity to diabetes. Diabetes Spectr. 2017;30(3):149-153. doi:10.2337/ds17-0011.
- Powers MA, Bardsley J, Cypress M, et al. Diabetes self-management education and support in type 2 diabetes: a joint position statement of the American Diabetes Association, the American Association of Diabetes Educators, and the Academy of Nutrition and Dietetics. Diabetes Care. 2015;38(7):1372-1382. doi:10.2337/dc15-0730.
- Van Gaal L, Scheen A. Weight management in type 2 diabetes: current and emerging approaches to treatment. Diabetes Care. 2015;38(6):1161-1172. doi:10.2337/dc14-1630.
- Puhl RM, Himmelstein MS, Hateley-Browne JL, Speight J. Weight stigma and diabetes stigma in U.S. adults with type 2 diabetes: associations with diabetes self-care behaviors and perceptions of health care. Diabetes Res Clin Pract. 2020;168:108387. doi:10.1016/j.diabres.2020.108387.
- Look AHEAD Research Group. Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes [published correction appears in N Engl J Med. 2014;370(19):1866]. N Engl J Med. 2013;369(2):145-154. doi:10.1056/NEJMoa1212914.
- Look AHEAD Research Group. Eight-year weight losses with an intensive lifestyle intervention: the Look AHEAD study. Obesity (Silver Spring). 2014;22(1):5-13. doi:10.1002/oby.20662.
- Redmon JB, Bertoni AG, Connelly S, et al. Effect of the Look AHEAD study intervention on medication use and related cost to treat cardiovascular disease risk factors in individuals with type 2 diabetes. Diabetes Care. 2010;33(6):1153-1158. doi:10.2337/dc09-2090.
- Melby C, Paris H, Foright R, Peth J. Attenuating the biologic drive for weight regain following weight loss: must what goes down always go back up? Nutrients. 2017;9(5):468. doi:10.3390/nu9050468.
- Lingvay I, Sumithran P, Cohen R, le Roux C. Obesity management as a primary treatment goal for type 2 diabetes: time to reframe the conversation. Lancet. 2022;399(10322):394-405. doi:10.1016/S0140-6736(21)01919-X.
- Sumithran P, Prendergast L, Delbridge E, et al. Long-term persistence of hormonal adaptations to weight loss. N Engl J Med. 2011:365(17):1597-1604. doi:10.1056/NEJMoa1105816.
- Thom G, McIntosh A, Messow CM, et al. Weight loss-induced increase in fasting ghrelin concentration is a predictor of weight regain: evidence from the Diabetes Remission Clinical Trial (DiRECT). Diabetes Obes Metab. 2021;23(3):711-719. doi:10.1111/dom.14274.
- Lean MEJ, Leslie WS, Barnes AC, et al. Durability of a primary care-led weight-management intervention for remission of type 2 diabetes: 2-year results of the DiRECT open-label, cluster-randomised trial. Lancet Diabetes Endocrinol. 2019;7(5);344-355. doi:10.1016/S2213-8587(19)30068-3.
- Nunes CL, Jesus F, Francisco R, et al. Adaptive thermogenesis after moderate weight loss: magnitude and methodological issues. Eur J Nutr. 2021;61(3):1405-1416. doi:10.1007/s00394-021-02742-6.
- Lien LF, Haqq AM, Arlotto M, et al. The STEDMAN project: biophysical, biochemical and metabolic effects of a behavioral weight loss intervention during weight loss, maintenance, and regain. OMICS. 2009;13(1):21-35. doi:10.1089/omi.2008.0035.
- Alberti KGMM, Eckel RH, Grundy SM, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120(16):1640-1645.
- Davies MJ, Aroda VR, Collins BS, et al. Management of hyperglycemia in type 2 diabetes, 2022. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2022;45(11):2753-2786. doi.org/10.2337/dci22-0034.
- Gregg EW, Chen H, Wagenknecht LE, et al. Association of an intensive lifestyle intervention with remission of type 2 diabetes. JAMA. 2012;308(23):2489-2496. doi:10.1001/jama.2012.67929.
- Apovian C, Okemah J, O’Neil P. Body weight considerations in the management of type 2 diabetes. Adv Ther. 2019:36:44-58. doi.org/10.1007/s12325-018-0824-8.