Let’s TALK!
Navigating sensitive conversations about weight to support T2D management can be challenging for both HCPs and patients. For examples of collaborative and effective conversations, watch this series of short videos focused on Assessing patient readiness, Advising and educating patients, and Acknowledging the challenges to support patients in their diabetes care journeys.
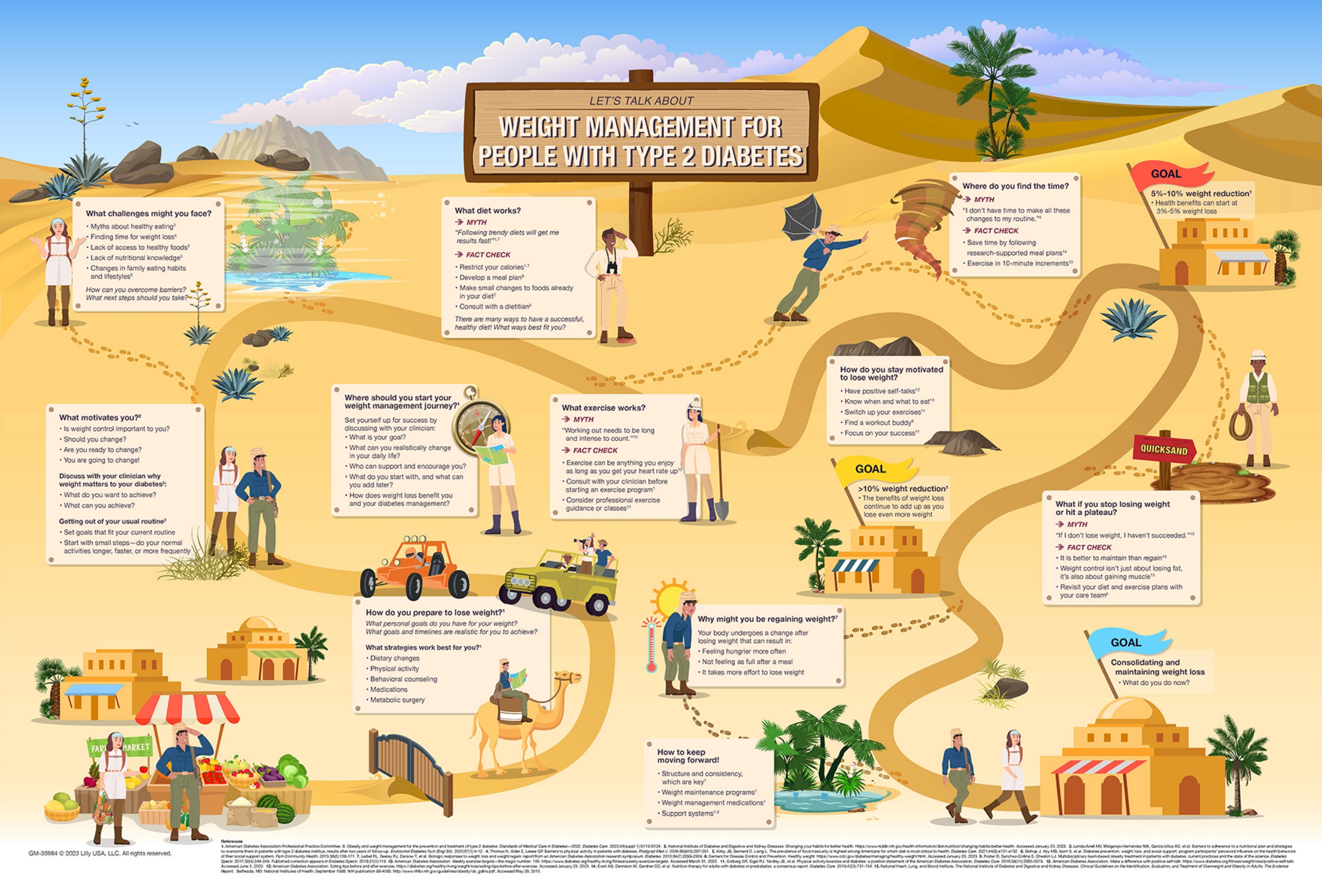
Medical Workmat
Conversations about weight management in patients with T2D can be challenging. Download the Medical Workmat to help navigate those conversations.
DOWNLOAD
Additional support
The following resources may be helpful when addressing and managing weight in T2D. These resources are not developed by Eli Lilly and will direct you to an external site.
RESOURCES FOR CLINICIANS
How to Approach Conversations About A1C and Weight:
ADA Resources:
Ethnic Differences in BMI:
RESOURCES FOR PATIENTS WITH T2D
ADA Resources:
How to Correctly Measure Waist Circumference:
Body-Weight Planner:
BMI Calculator:
References
- UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998;352(9131):837-853.
- Holman RR, Paul SK, Bethel MA, et al. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008;359(15):1577-1589.
- Cheng Y-H, Tsao Y-C, Tzeng I-S, et al. Body mass index and waist circumference are better predictors of insulin resistance than total body fat percentage in middle-aged and elderly Taiwanese. Medicine (Baltimore). 2017;96(39):e8126.
- Racette SB, Evans EM, Weiss EP, Hagberg JM, Holloszy JO. Abdominal adiposity is a stronger predictor of insulin resistance than fitness among 50-95 year olds. Diabetes Care. 2006;29(3):673-678.
- Chait A, den Hartigh LJ. Adipose tissue distribution, inflammation and its metabolic consequences, including diabetes and cardiovascular disease. Front Cardiovasc Med. 2020;7:22.
- Trouwborst I, Bowser SM, Goossens GH, Blaak EE. Ectopic fat accumulation in distinct insulin resistant phenotypes; targets for personalized nutritional interventions. Front Nutr. 2018;5:77.
- de Luca C, Olefsky JM. Inflammation and insulin resistance. FEBS Lett. 2008;582(1):97-105.
- Ye R, Onodera T, Scherer PE. Lipotoxicity and β cell maintenance in obesity and type 2 diabetes. J Endocr Soc. 2019;3(3):617-631.
- Sobczak AIS, Blindauer CA, Stewart AJ. Changes in plasma free fatty acids associated with type-2 diabetes. Nutrients. 2019;11(9):2022.
- DeFronzo RA. Banting lecture. From the triumvirate to the ominous octet: a new paradigm for the treatment of type 2 diabetes mellitus. Diabetes. 2009;58(4):773-795.
- American Diabetes Association Professional Practice Committee. 5. Facilitating Positive Health Behaviors and Well-being to Improve Health Outcomes: Standards of Care in Diabetes—2024. Diabetes Care. 2024;47(suppl 1):S77-110. doi:10.2337/dc24-S005.
- Tucker S, Bramante C, Conroy M, et al. The most undertreated chronic disease: addressing obesity in primary care settings. Curr Obes Rep. 2021;10(3):396-408.